SURGERY
WINDOW OF OPPORTUNITY
AND PATHOLOGY
SURGERY - WINDOW OF OPPORTUNITY
EDITORS' NOTE
BEFORE SURGERY: "The waiting period to surgery represents a valuable 'window of opportunity' to evaluate novel therapeutic strategies." Arnaout A et al., 2015.
AROUND SURGERY: "We have found that perioperative anti-inflammatory agents appear to abrogate the early hazard of recurrence, and we estimate that such intervention could reduce breast cancer mortality by 25-50%." Retsky M et al., 2012.
AFTER SURGERY: "We propose a novel therapeutic paradigm; that the postoperative period represents a window of opportunity during which the patient may be further protected against the oncological effects of tumor
removal." Coffey JC et al., 2003.
The thrust of this SURGERY-WINDOW OF OPPORTUNITY section is to share an article and many studies that compellingly convey both old and new research finding that surgery is hugely damaging, and that steps must be taken to ameliorate this harm. Thus, the period between the initial biopsy and surgery, or if you don't have a biopsy, the period revolving around the time of the actual surgery, offer a window of opportunity for the breast cancer patient to implement strategies to mitigate the harm.
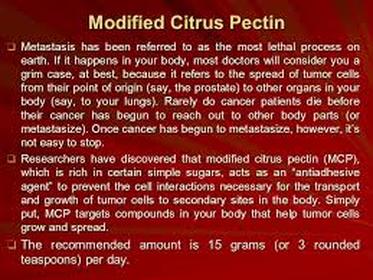
The strategies invoked by the various researchers mostly aim to quell the inflammation attendant to the surgery. Hence, NSAIDS (non-steroidal anti-inflammatory drugs) have been invoked either prior to or even during surgery, itself, such as etodolac, diclofenac, and ketorolac. Michael Retsky, PHD, hypothesizes that ketorolac could cut early breast cancer relapse by 50%. And there is propranolol, a beta-blocker, to calm nervousness (catecholamines). Plus, such things as modified citrus pectin and the whole apple pectin may be useful to prevent surgery-induced cell adhesion.
EDITORS' NOTE
BEFORE SURGERY: "The waiting period to surgery represents a valuable 'window of opportunity' to evaluate novel therapeutic strategies." Arnaout A et al., 2015.
AROUND SURGERY: "We have found that perioperative anti-inflammatory agents appear to abrogate the early hazard of recurrence, and we estimate that such intervention could reduce breast cancer mortality by 25-50%." Retsky M et al., 2012.
AFTER SURGERY: "We propose a novel therapeutic paradigm; that the postoperative period represents a window of opportunity during which the patient may be further protected against the oncological effects of tumor
removal." Coffey JC et al., 2003.
The thrust of this SURGERY-WINDOW OF OPPORTUNITY section is to share an article and many studies that compellingly convey both old and new research finding that surgery is hugely damaging, and that steps must be taken to ameliorate this harm. Thus, the period between the initial biopsy and surgery, or if you don't have a biopsy, the period revolving around the time of the actual surgery, offer a window of opportunity for the breast cancer patient to implement strategies to mitigate the harm.
The strategies invoked by the various researchers mostly aim to quell the inflammation attendant to the surgery. Hence, NSAIDS (non-steroidal anti-inflammatory drugs) have been invoked either prior to or even during surgery, itself, such as etodolac, diclofenac, and ketorolac. Michael Retsky, PHD, hypothesizes that ketorolac could cut early breast cancer relapse by 50%. And there is propranolol, a beta-blocker, to calm nervousness (catecholamines). Plus, such things as modified citrus pectin and the whole apple pectin may be useful to prevent surgery-induced cell adhesion.
Between the biopsy and surgery, or if you are just going to have the tumor removed all at once (that the EDITORS recommend), there are many natural items to consider. How about considering taking ginger, quercetin, and bromelain for inflammation? How about the Bach Flower formula, Rescue Remedy, for anxiety? How about eating only organic food (FOODS' section)? Taking anti-parasite herbs (HERBS AND SUPPLEMENTS' section)? Doing oxidative therapies (OZONE section)? Using electronic devices (FREQUENCIES' section)? And do check out Frenkel M et al.'s "window of therapeutic opportunity" in the HOMEOPATHY section,
What a powerful perioperative window of opportunity!
PLEASE CONSULT WITH YOUR MEDICAL PROFESSIONALS AS TO WHEN TO STOP USING ANY NATURAL THERAPY AS THERE COULD BE A CONFLICT, SUCH AS BLEEDING, DURING THE SURGERY.
PLEASE CONSULT WITH YOUR MEDICAL PROFESSIONALS AS TO WHEN TO STOP USING ANY NATURAL THERAPY AS THERE COULD BE A CONFLICT, SUCH AS BLEEDING, DURING THE SURGERY.
SURGERY - WINDOW OF OPPORTUNITY
MINIMAL RESIDUAL DISEASE" IS LEFT AFTER CANCER SURGERY - TUMOR REMOVAL ALTERS THE GROWTH OF RESIDUAL DISEASE, leading TO "PERIOPERATIVE TUMOR GROWTH". = NEED TO PROTECT THE CANCER PATIENT!
BACKGROUND
"Excisional surgery is one of the primary treatment modalities for cancer. Minimal residual disease is the occult neoplastic disease that remains in situ after curative surgery. There is increasing evidence that tumor removal alters the growth of minimal residual disease, leading to perioperative tumor growth. ... We propose a novel therapeutic paradigm that the postoperative period represents a window of opportunity during which the patient may be further protected against the oncological effects of tumor removal."
Coffey JC et al., The Perioperative Period is an Underutilized Window of Therapeutic Opportunity in Patients with Colorectal Cancer, Lancet Oncol., 2003.
Coffey JC et al., The Perioperative Period is an Underutilized Window of Therapeutic Opportunity in Patients with Colorectal Cancer, Lancet Oncol., 2003.
WINDOW OF OPPORTUNITY
BEFORE BREAST CANCER SURGERY: HOW TO PROTECT THE PATIENT 2015 STUDY! GIVING BIOPSY DIAGNOSED BREAST CANCER PATIENTS AN AROMATASE INHIBITOR, ANASTROZOLE, FOR A MEAN PERIOD OF 24.7 DAYS BEFORE SURGERY LED TO SIGNIFICANT DECLINE IN PROLIFERATION, ALTHOUGH NOT APOPTOSIS - FEASIBILITY OF WINDOW OF OPPORTUNITY STUDIES!
"The waiting period to surgery represents a valuable 'window of opportunity' to evaluate novel therapeutic strategies."
In the Arnaout A et al. 2015 study, the researchers gave biopsy-diagnosed breast cancer patients the aromatase inhibitor, anastrozole, for a mean period of 24.7 days before their breast cancer surgery and assessed proliferation and apoptosis rates before and after surgery.
Results: "There were a statistically significant decline in mean Ki67 (a marker of proliferation) indices of 48.8% and a trend towards significance in the decline of CC3 (a marker of apoptosis) when comparing pre- with post- treatment values." It is great that Ki67 proliferation rate declined, but why the decrease in apoptosis? The researchers commented that a decrease in apoptosis has been seen in endocrine therapy, perhaps because "the capacity of breast cancer cells to pass into apoptosis is retarded by the profound antiproliferative effects of antiestrogenic therapy".
Conclusion: "Window of opportunity trials in breast cancer are a feasible way of assessing the biologic efficacy of different therapies in the presurgical setting."
(See Arnaout A et al., Evaluating the Feasibility of Performing Window of Opportunity Trials in Breast Cancer, International Journal of Surgical Oncology, 2015.)
"The waiting period to surgery represents a valuable 'window of opportunity' to evaluate novel therapeutic strategies."
In the Arnaout A et al. 2015 study, the researchers gave biopsy-diagnosed breast cancer patients the aromatase inhibitor, anastrozole, for a mean period of 24.7 days before their breast cancer surgery and assessed proliferation and apoptosis rates before and after surgery.
Results: "There were a statistically significant decline in mean Ki67 (a marker of proliferation) indices of 48.8% and a trend towards significance in the decline of CC3 (a marker of apoptosis) when comparing pre- with post- treatment values." It is great that Ki67 proliferation rate declined, but why the decrease in apoptosis? The researchers commented that a decrease in apoptosis has been seen in endocrine therapy, perhaps because "the capacity of breast cancer cells to pass into apoptosis is retarded by the profound antiproliferative effects of antiestrogenic therapy".
Conclusion: "Window of opportunity trials in breast cancer are a feasible way of assessing the biologic efficacy of different therapies in the presurgical setting."
(See Arnaout A et al., Evaluating the Feasibility of Performing Window of Opportunity Trials in Breast Cancer, International Journal of Surgical Oncology, 2015.)
WINDOW OF OPPORTUNITY
BEFORE BREAST CANCER SURGERY: HOW TO PROTECT THE PATIENT? 2015 STUDY: DIABETES DRUG, METFORMIN, PRIOR TO SURGERY INDUCES FALLS IN CELL PROLIFERATION AND "SUPPRESSION OF INSULIN RESPONSES".
In the Hadad SM et al. 2015 study, the researchers "examined biomarker effects of the diabetes drug, Metformin, in primary breast cancer in a preoperative window of opportunity trial".
In this study, the breast cancer patients were given 500 mg daily of Metformin for a week, then 1 gram twice daily for a further week. A core biopsy was conducted before the surgery and then during the surgery.
Results of Taking Metformin: There was up-regulation of pAMPk (metabolism master - uptake of insulin) and down-regulation of pAKt (inhibitor of apoptosis). There were falls in Ki 67 (cell proliferation) and cleaved caspase-3.
"These biomarker data suggest mechanisms for Metformin action in vivo in breast cancer patients via up-regulation of tumor pAMPK, down-regulation of pAkt, and suppression of insulin responses."
(See Hadad SM et al., Evidence for Biological Effects of Metformin in Operable Breast Cancer; Biomarker Analysis in a Pre-Operative Window of Opportunity Randomized Trial, Breast Cancer Res Treat, 2015.)
WINDOW OF OPPORTUNITY
BEFORE BREAST CANCER SURGERY: HOW TO PROTECT THE PATIENT?
THE NSAID, ETODOLAC, 400 MG TWICE A DAY UNTIL TWO DAYS BEFORE SURGERY. CYCLIN D1 DECREASED (CELL CYCLE PROGRESSION!), BUT INCREASE IN COX-2 PATHWAY (COMPENSATORY MECHANISM FOR COX-2?)
" Nonsteroidal anti-inflammatory drugs (NSAIDs) are cyclooxygenase (COX)-1 and -2 inhibitors that are commonly used to treat pain, inflammation, and fever. In large epidemiological studies, NSAID use has been associated with a preventive effect in breast cancer.. Overexpression of COX-2 in cancer is known to promote tumor growth via stabilization and nuclear translocation of β-catenin which then leads to expression of growth-promoting genes."
In the Schwab R et al. "window of opportunity" 2015 study, the researchers evaluated the NSAID, etodolac, on breast cancer markers.
Breast cancer patients took etodolac 400 mg orally twice daily after a diagnosis of breast cancer via biopsy, and continued to take the etodolac until two days before surgery. Tumor specimens taken BEFORE and AFTER surgery were evaluatated for "COX-2 and B-catenin, and the RXRα pathway (RXRα, PPARγ, and cyclin D1 ) as well as cyclin D1 protein level". (Note that, "Cyclin D1 is a member of the cyclin protein family that is involved in regulating cell cycle progression." -wikipedia.org.).
Before and after etodolac exposure: Etodolac is associated with a decrease in cyclin D1 protein level, especially after taking it longer. This is good, because cyclin D is involved in cell cycle progression. "We also observed an increase in COX-2 pathway (COX-2 and possibly β-catenin) gene expression after etodolac exposure. Although etodolac is a well-known selective COX-2 enzymatic inhibitor, compensatory increased gene expression of COX-2 with NSAIDs has been reported in the past . Additional study, such as analysis of prostaglandin E2 levels, will be required to determine if the increased gene expression level of COX-2 after etodolac exposure is associated with preserved enzymatic activity."
Conclusion: "Assay of a limited set of rationally identified genes, evaluated before and after etodolac exposure, found that etodolac is associated with a decrease in cyclin D1 protein level as assayed by immunohistochemistry." Note that the increase in COX-2 pathway needs further exploration." (See Schwab R et al., A Window-of-Opportunity Biomarker Study of Etodolac in Resectable Breast Cancer, Cancer Medicine, 2015.)
............ON TO ANOTHER STUDY USING THE COX-2 INHIBITOR, ETODOLAC....
WINDOW OF OPPORTUNITY
BEFORE BREAST CANCER SURGERY: HOW TO PROTECT THE PATIENT? USE A BETA BLOCKER, PROPRANOLOL, AND A COX-2 INHIBITOR, ETODOLAC
"Here we argue that the short perioperative periiod is disproportionately critical in determining long-term recurrence rates, discuss the various underlying risk factors that act synergistically during this period, and assert that this time frame presents an unexplored opportunity to reduce long-term cancer recurrence."
Neeman E et al., 2012.
In the Neeman E et al. 2012 study, the thrust of the research was on the "excess perioperative release of catecholamines and prostaglandins, which were recently shown to be prominent in facilitating cancer recurrence through their direct impact on the malignant tissue and its microenvironment, and through suppressing antimetastatic immunity".
What are catecholamines? Catecholamines, such as dopamine, norepinephrine, and epinephrine (adrenalin), "are commonly elevated perioperatively. ... Catecholamines are abundantly released throughout the perioperative period, due to the patients' anxiety and fear of the disease..."
What are prostaglandins? Hormone-like, prostaglandins, among many things, modulate inflammation. Tumors and/or recruited macrophages release prostaglandins as an immune escape or to propel vascularization. Similarly, surgery-damaged tissues release prostaglandins.
"Interestingly, many human malignancies express receptors for catecholamines and prostaglandins, and almost all leukocytes express both receptor systems. Thus, it is reasonable to assume that both immune and tumor cells are affected by catecholamines and prostaglandins, which are simultaneously elevated during the perioperative period."
Proposal: Use a β-blocker (propranolol) to help with the inhibition of catecholamines and, for prostaglandins, a COX2-inhibitor (etodolac),
Why? "(i) The disproportional impact of the short perioperative period in determining long-term cancer outcomes; (ii) the recent discovery of leukocyte populations that can control tumor progression, provided protection from immunosuppression; (iii) the recent findings that excess catecholamine and prostaglandin secretions underlie many of the perioperative risk factors for long-term recurrence, through immune suppression and through nonimmunological mechanisms; and (iv) the few positive findings in animal and human studies employing each drug alone,, and the promising results from our animal studies employing the combined blockade of catecholamines and prostaglandins."
When? "The drug treatment should commence a few days prior to surgery, as psychological distress and malignant tissue (and its surrounding stromal and immune cells) are known to induce the release of catecholamines and prostaglandins, respectively, even before surgery when immune-suppression has been reported."
(See Neeman E et al., A New Approach to Reducing postsurgical Cancer Recurrence: Perioperative Targeting of Catecholamines and prostaglandins, Clin Cancer Rese, 2012.)
WINDOW OF OPPORTUNITY
BEFORE BREAST CANCER SURGERY - HOW TO PROTECT THE PATIENT? THE NSAID, KETOROLAC, RECOMMENDED TO QUELL INFLAMMATION, HALT METASTASIS - RETSKY THEORY: COULD CUT UP TO 50% EARLY RELAPSE!
Drawing upon 2010 Forget P et al.'s retropspective study of intraoperative ketorolac for mastectomies that helped reduce early relapse, Retsky's THEORY is that taking the NSAID, ketorolac, before surgery to quell the inflammation could possibly cut in half the early relapse rate from breast cancer. ..... "The startling result was that one low cost drug- the non steroidal anti-inflammatory (NSAID) ketorolac – was strongly associated with far better four year breast cancer outcome than any of the other three non-NSAID analgesics (sufentanil, clonidine, and ketamine)."
In a 2014 You Tube presentation, Michael Retsky, PHD, stated that after breast cancer surgery, there is "transient inflammation for about a week".
Retsky's THEORY is that taking the NSAID, ketorolac, before surgery to quell the inflammation could possibly cut in half the early relapse rate from breast cancer. But this is just a theory. This is the same Retsky who likely caused consternation in the mammography world when he found Italian "data that suggests surgery-induced angiogenesis for premenopausal node positive patients would produce 1 early relapse per 10,000 persons age 40-49 who were screened for early detection." (See the BIOPSY section.)
Of late, he has been pondering how to curtail cancer metastasis, and his focus has been on ketorolac.
Cancer does not follow a strict path of growth. Metastatic disease is mostly inactive prior to surgery, but is some how propelled to grow after surgery.
"Most relapses in breast cancer would fall into the surgery-induced growth category."
On to attempting to curtail the metastasis ...
Upon reading the 2010 Forget P et al. retropspective study of intraoperative ketorolac for mastectomies that helped reduce early relapse, the Retsky et al. 2012 study "independently re-examined and updated their data and, in search of a mechanism, focused in on the transient systemic inflammation that follows surgery to remove a primary tumor".
How would the anti-inflammatory, ketorolac, be helpful? Mechanically, "Capillary leakage from transient systemic inflammation as a result of the surgery in the presence of circulating cancer cells and cells released during surgery and resulting inflammatory oncotaxis is blocked by directly preventing the inflammation. This prevents single cell activation." Biologically, tumor removal "directly or indirectly elicits peritumoral endothelial cell proliferation.. A) Angiogenic factors, like VEGF and bFGF, are directly released or even produced via IL-6; B) Bone marrow derived CXCR-4 positive cells, acting both on tumor foci and on the inflammatory process, are mobilized by SDF-1, directly released or even produced via COX-2. ... In addition, NSAIDS have antiangiogenic properties; thus, surgery-induced angiogenesis is prevented."
Conclusion: "The startling result was that one low cost drug- the non steroidal anti-inflammatory (NSAID) ketorolac – was strongly associated with far better four year breast cancer outcome than any of the other three non-NSAID analgesics (sufentanil, clonidine, and ketamine). The early relapses that we have associated with surgery are all but absent among patients who had been given perioperative ketorolac."
(See Retsky M et al., Promising Development from Translational or Perhaps Anti-Translational Research in Breast Cancer, Clin Trans Med, 2012. For the You Tube, https://www.youtube.com/watch?v=LMRiuagnLQk/)
WINDOW OF OPPORTUNITY
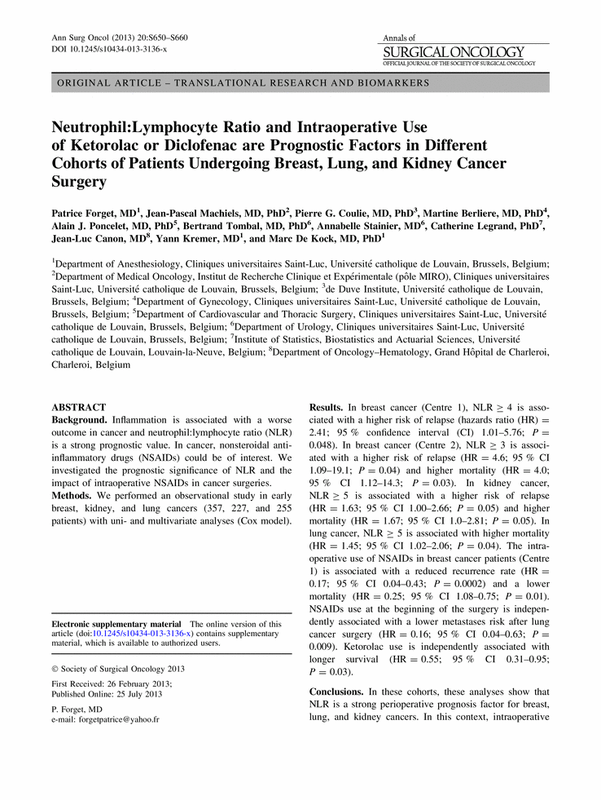
DURING BREAST CANCER SURGERY: HOW TO PROTECT THE PATIENT? - SINGLE DOSE OF NSAIDS (EITHER KETOROLAC OR DICLOFENAC) DURING SURGERY FOR LUMPECTOMY IS ASSOCIATED WITH IMPROVED DISEASE-FREE SURVIVAL AND OVERALL SURVIVAL
|
In the Forget P et al. 2014 study, the researchers conducted a retrospective study on "the effect of a single intraoperative dose of ketorolac or diclofenac, and the preoperative neutrophil:lymphocyte ratio during conservative primary breast cancer surgery, on disease-free survival". Findings: The single intraoperative use of NSAIDS (ketorolac and diclofenac) improved the disease free survival, along with improved overall survival. Those breast cancer patients having a neutrophil:lymphocyte ratio over 3.3 had a shorter disease free survival. Conclusion for Lumpectomy Surgery: "Intraoperative NSAIDs and higher preoperative neutrophil:lymphocyte ratio are associated with improved outcome in conservative breast cancer surgery." (See Forget P et al., Intraoperative Use of Ketorolac or Diclofenac is Associated with Improved Disease-Free Survival and Overall Survival in Conservative Breast Cancer Surgery, Br J Anesth, 2014.) |
WINDOW OF OPPORTUNITY
POST-SURGERY: HOW TO PROTECT THE PATIENT? WONDERFUL ARTICLE: PREVENTING SURGERY-INDUCED CANCER METASTASIS, BY STEVEN NEMEROFF, ND, 2009 -MODIFIED CITRUS PECTIN (MCP) FOR CELL ADHESION
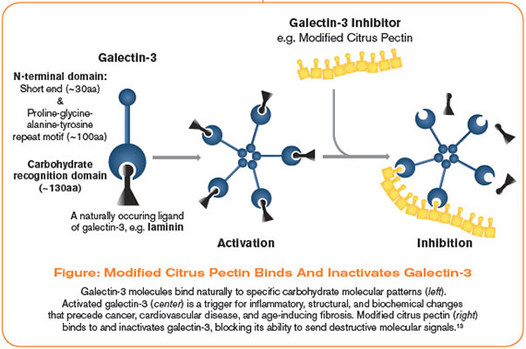
Steven Nemeroff, ND, wrote a terrrific, extensive article about preventing surgery-induced cancer metastasis in Life Extension. One of the many items he comprehensively wrote about that will be helpful to prevent surgery-induced metastasis is modified citrus pectin (MCP).
Dr. Nemeroff wrote, "Regrettable research has shown that cancer surgery increases tumor cell adhesion. In one experiment that mimicked surgical conditions, scientists reported that the binding of cancer cells to the blood vessel walls was increased by 250%, compared to cancer cells not exposed to surgical conditions. Therefore, it is critically important for the person undergoing cancer surgery to take measures that can help to neutralize the surgery-induced increase in cancer cell adhesion. Fortunately, a natural supplement called modified citrus pectin (MCP) can do just that. Citrus pectin - a type of dietary fiber - is not absorbed from the intestine. However, modified citrus pectin has been altered so that it can be absorbed into the blood and exert its anti-cancer effects. The mechanism by which modified citrus pectin inhibits cancer cell adhesion is by binding to galectin-3 adhesion molecules on the surface of cancer cells, thereby preventing cancer cells from sticking together and forming a cluster. Modified citrus pectin can also inhibit circulating tumor cells from latching onto the lining of blood vessels. This was demonstrated by an experiment in which modified citrus pectin blocked the adhesion of galectin-3 to the lining of blood vessels by an astounding 95%. Modified citrus pectin also substantially decreased the adhesion of breast cancer cells to the blood vessel walls."
(See Steven Nemeroff, ND, Preventing Surgery-Induced Cancer Metastasis, Life Extension, 2009. http://www.lifeextension.com/Magazine/2009/12/Preventing-Surgery-Induced-Cancer-Metastasis/Page-01.)
UNMODIFIED APPLE PECTIN
2015 STUDY: UNMODIFIED APPLE PECTIN HELPFUL FOR ESTROGEN NEGATIVE CELLS TO INHIBIT CELL GROWTH AND REDUCE CELL ATTACHMENT
In the above cited article, we learned that modified citrus pectin may help prevent cell adhesion attendant to surgery.
How about unmodified pectic acid from apples?
"Apples and citrus fruits are the main sources of pectin which can be applied for anti-cancer research."
In the Delphi L et al., 2015 study, the researchers investigated.."pectic acid, a type of pectic oligoshacharide (a D-galacturonic acid), from apples" on estrogen-negative breast cancer cells.
Results: "The results indicated that pectic acid inhibited cell growth and reduced cell attachment after 24 hours incubation. ... This study indicated that pectic acid in its intact form caused growth inhibition correlated with cell death and apoptosis induction in breast cancer cells." Note that the heat modified form of pectic acid did not intensify the effects in the estrogen-negative breast cancer cells. "Thus, intact pectic acid might improve cancer therapy quality without worrying about long-term administration and side effects, as pectic acid originates from fruit."
Conclusion: These data indicate that apple pectic acid without any modification could trigger apoptosis in estrogen- negative breast cancer cells and has potential to improve cancer treatment as a natural product."
(See Delphi L et al., Pectic-Oligoshaccharides from Apples Induce Apoptosis and Cell Cycel Arrest in MDA-MB-231 Cells, a Model of Human Breast Cancer, Asian Pacific Journal of Cancer Prevention, 2015.)
WINDOW OF OPPORTUNITY
FOR PREMENOPAUSAL WOMEN, TIMING OF SURGERY DURING MENSTRUAL CYCLE? TIMING SURGERY STILL REMAINS CONTROVERSIAL
NO EFFECT SEEN IN THREE YEAR PROSPECTIVE STUDY
In the Thorpe H et al. 2008 study, the researchers did a prospective three-year study to see if timing of breast cancer surgery would have any effect on the patients' survival.
The researchers concluded that the timing of the surgery had no effect on the prognosis. There had been a hint in the Hrushesky et al. 1989 study that perimenstrual surgery worsened both disease free and overall survival rates. However, the Thorpe group found that, .. "Timing of breast cancer surgery in relation to the menstrual cycle phase had no significant impact on 3-year survival in this study. This may be due to almost all patients receiving some form of adjuvant therapy. Longer-term analysis will be performed at 10 years when all patients have reached this follow-up. This will allow us to obtain a definitive answer to the controversial question of the effect of timing of surgery with respect to patients' menstrual cycle phase on prognosis."
EDITORS' NOTE: The Joshi PA et al. 2010 study found that in the reproductive cycle of mice - when progesterone peaks - there is a 14-fold increase in the number of mammary stem cells during what would be our human luteal latter phase. The impact? The Joshi group stated that cross-talk between stem cells and neighboring breast cells that propels an expansion of stem cells may trigger an environment where cancer can begin. So, it does not seem to be an auspicious start to have breast cancer surgery during the latter part of the cycle, does it?
(For the Thorpe study, see Thorpe H et al. Timing of Breast Cancer Surgery in Relation to Menstrual Cycle Phase: No Effect on 3-Year Prognosis: The ITS Study, Br J Cancer, 2008. ...For the Joshi study, see Joshi PA et al., Progesterone Induces Adult Mammary Stem Cell Expansion, Nature, 2006.)
SURGERY - PATHOLOGY - AFTER SURGERY COMES THE PATHOLOGY REPORT
BACKGROUND - SO, YOU'VE HAD SURGERY. WHAT DOES THE PATHOLOGY REPORT MEAN? SOME FINDINGS THAT MIGHT BE REFLECTED ON YOUR PATHOLOGY REPORT - EXCERPTS FROM AMERICAN CANCER SOCIETY
IN SITU TUMORS: "Carcinoma is a term used to describe a cancer that begins in the lining layer (epithelial cells) of organs like the breast. Nearly all breast cancers are carcinomas. ... As long as the carcinoma cells are still confined to the breast ducts or lobules, without breaking out and growing into surrounding tissue, it is considered in-situ carcinoma."
INVASIVE TUMORS THAT CAN SPREAD: "Once the carcinoma cells (mostly ductal and lobular) have grown and broken out of the ducts or lobules, it is called invasive or infiltrating carcinoma... In invasive ductal carcinoma, the most common type of breast cancer, the cancer seems to have started in a duct (milk passage), and then grown through the wall of the duct into the fatty tissue of the breast. In invasive lobular carcinoma, the cancer seems to have started in the lobule, and then grown through the wall of the duct into the fatty tissue of the breast."
DIFFERENTIATION: "Well-differentiated carcinomas have relatively normal-looking cells that do not appear to be growing rapidly and are arranged in small tubules for ductal cancer and cords in lobular cancer. These cancers tend to grow and spread slowly and so have a better prognosis (outlook). Poorly differentiated carcinomas lack normal features, tend to grow and spread faster, and have a worse prognosis."
CANCER DIVISION "Ki67 is a way to measure how fast the cancer cells are growing and dividing. High values (over 30%) for Ki67 mean that many cells are dividing, and predict a poorer prognosis (outlook)."
STAGING: Cancer staging is based upon such things as tumor size and number of lymph nodes involved. "Staging is expressed in Roman numerals from stage I (the least advanced stage) to stage IV (the most advanced stage). Non-invasive cancer is listed as stage 0."
HORMONE RECEPTORS: "Receptors are proteins on the outside surfaces of cells that can attach to certain substances, such as hormones, that circulate in the blood. Normal breast cells and some breast cancer cells have receptors that attach to estrogen and progesterone. ... Breast cancers that contain estrogen receptors are often referred to as ER-positive (or ER+) cancers, while those containing progesterone receptors are called PR-positive (or PR+) cancers. Women with hormone receptor–positive cancers tend to have a better prognosis and are much more likely to respond to hormone therapy than women with cancers without these receptors."
HER2: "About 1 of 5 breast cancers have too much of a growth-promoting protein called HER2/neu (often just shortened to HER2). ...Women with HER2-positive breast cancers have too many copies of the HER2/neu gene, resulting in greater than normal amounts of the HER2/neu protein. These cancers tend to grow and spread more aggressively than other breast cancers." (See American Cancer Society, http://www.cancer.org/treatment/understandingyourdiagnosis/understandingyourpathologyreport/breastpathology/breast-cancer-pathology.)
IN SITU TUMORS: "Carcinoma is a term used to describe a cancer that begins in the lining layer (epithelial cells) of organs like the breast. Nearly all breast cancers are carcinomas. ... As long as the carcinoma cells are still confined to the breast ducts or lobules, without breaking out and growing into surrounding tissue, it is considered in-situ carcinoma."
INVASIVE TUMORS THAT CAN SPREAD: "Once the carcinoma cells (mostly ductal and lobular) have grown and broken out of the ducts or lobules, it is called invasive or infiltrating carcinoma... In invasive ductal carcinoma, the most common type of breast cancer, the cancer seems to have started in a duct (milk passage), and then grown through the wall of the duct into the fatty tissue of the breast. In invasive lobular carcinoma, the cancer seems to have started in the lobule, and then grown through the wall of the duct into the fatty tissue of the breast."
DIFFERENTIATION: "Well-differentiated carcinomas have relatively normal-looking cells that do not appear to be growing rapidly and are arranged in small tubules for ductal cancer and cords in lobular cancer. These cancers tend to grow and spread slowly and so have a better prognosis (outlook). Poorly differentiated carcinomas lack normal features, tend to grow and spread faster, and have a worse prognosis."
CANCER DIVISION "Ki67 is a way to measure how fast the cancer cells are growing and dividing. High values (over 30%) for Ki67 mean that many cells are dividing, and predict a poorer prognosis (outlook)."
STAGING: Cancer staging is based upon such things as tumor size and number of lymph nodes involved. "Staging is expressed in Roman numerals from stage I (the least advanced stage) to stage IV (the most advanced stage). Non-invasive cancer is listed as stage 0."
HORMONE RECEPTORS: "Receptors are proteins on the outside surfaces of cells that can attach to certain substances, such as hormones, that circulate in the blood. Normal breast cells and some breast cancer cells have receptors that attach to estrogen and progesterone. ... Breast cancers that contain estrogen receptors are often referred to as ER-positive (or ER+) cancers, while those containing progesterone receptors are called PR-positive (or PR+) cancers. Women with hormone receptor–positive cancers tend to have a better prognosis and are much more likely to respond to hormone therapy than women with cancers without these receptors."
HER2: "About 1 of 5 breast cancers have too much of a growth-promoting protein called HER2/neu (often just shortened to HER2). ...Women with HER2-positive breast cancers have too many copies of the HER2/neu gene, resulting in greater than normal amounts of the HER2/neu protein. These cancers tend to grow and spread more aggressively than other breast cancers." (See American Cancer Society, http://www.cancer.org/treatment/understandingyourdiagnosis/understandingyourpathologyreport/breastpathology/breast-cancer-pathology.)
YOU RECEIVED YOUR PATHOLOGY REPORT
NEED A SECOND OPINION?
"...Patients with node-negative breast cancer or DCIS may represent a particularly relevant subgroup to consider for routine pathology review. It should be recognized that differences in interpretation among pathologists make it difficult to definitely determine the correct opinion. Review remains relevant in the era of gene expression signatures (note - such as Oncotype DX) to determine margin and nodal status, which may result in significant changes in systemic radiation, or surgical management. The findings emphasize the relavance of accurate pathology, which can not be substituted by a gene expression array. The reported rates of change on review are significant enough to warrant targeted review this this patient population and highlight the value of secondary review of pathology materials before final treatment is recommended." Kennecke HF et al., 2012.
NEED A SECOND OPINION?
"...Patients with node-negative breast cancer or DCIS may represent a particularly relevant subgroup to consider for routine pathology review. It should be recognized that differences in interpretation among pathologists make it difficult to definitely determine the correct opinion. Review remains relevant in the era of gene expression signatures (note - such as Oncotype DX) to determine margin and nodal status, which may result in significant changes in systemic radiation, or surgical management. The findings emphasize the relavance of accurate pathology, which can not be substituted by a gene expression array. The reported rates of change on review are significant enough to warrant targeted review this this patient population and highlight the value of secondary review of pathology materials before final treatment is recommended." Kennecke HF et al., 2012.
2016 STUDY ON VARIABILITY OF PATHOLOGISTS' OPINIONS
In the Elmore J et al 2016 study, there was a 75% concordance of opinions among pathologists on breast biopsies.
Most of the agreement was on invasive breast cancer. However, there was more disagreement on benign findings, such as atypia or DCIS. What is troubling is that these benign conditions need to be watched, as there is a possibility that they can progress to invasive breast cancer.
Commenting on the study, Anna Azvolinsky, for Cancer Network, wrote, "Of the slides of benign tissue, 87% were concordant and 13% of the samples were overinterpreted. The concordance rate was 96% for samples containing invasive carcinoma with a 4% underinterpretation rate. Of the atypical hyperplasia samples, the concordance rate among pathologists was 48%; 17% of the samples were overinterpreted and 35% of the samples were underinterpreted. The concordance rate was 84% for DCIS; 3% of the samples were overinterpreted and 13% were underinterpreted."
The study concluded: "This analysis, based on interpretation of a single breast biopsy slide per case, predicts a low likelihood that a diagnosis of atypia or DCIS would be verified by a reference consensus diagnosis."
For the article, see Anna Azvolinsky, 2015, http://www.cancernetwork.com/breast-cancer/pathologists-often-disagree-breast-biopsy-findings#sthash.SY8ntyH4.dpuf. For the study, see Elmore J et al., Variability in Patholigsts interpretation of Individual Biopsy Slides: A Population Perspective, Annals of Internal medicine, 2016.
In the Elmore J et al 2016 study, there was a 75% concordance of opinions among pathologists on breast biopsies.
Most of the agreement was on invasive breast cancer. However, there was more disagreement on benign findings, such as atypia or DCIS. What is troubling is that these benign conditions need to be watched, as there is a possibility that they can progress to invasive breast cancer.
Commenting on the study, Anna Azvolinsky, for Cancer Network, wrote, "Of the slides of benign tissue, 87% were concordant and 13% of the samples were overinterpreted. The concordance rate was 96% for samples containing invasive carcinoma with a 4% underinterpretation rate. Of the atypical hyperplasia samples, the concordance rate among pathologists was 48%; 17% of the samples were overinterpreted and 35% of the samples were underinterpreted. The concordance rate was 84% for DCIS; 3% of the samples were overinterpreted and 13% were underinterpreted."
The study concluded: "This analysis, based on interpretation of a single breast biopsy slide per case, predicts a low likelihood that a diagnosis of atypia or DCIS would be verified by a reference consensus diagnosis."
For the article, see Anna Azvolinsky, 2015, http://www.cancernetwork.com/breast-cancer/pathologists-often-disagree-breast-biopsy-findings#sthash.SY8ntyH4.dpuf. For the study, see Elmore J et al., Variability in Patholigsts interpretation of Individual Biopsy Slides: A Population Perspective, Annals of Internal medicine, 2016.
You want another opinion on your surgical pathology report. What exactly is a second opinion?
EXAMPLE: EXCERPTS FROM JOHNS HOPKINS PATHOLOGY DEPARTMENT
SECOND OPINIONS FOR BREAST TUMORS
SECOND OPINIONS FOR BREAST TUMORS
- "Cancer or Benign. In some cases, it may be very difficult to be sure if a breast lesion is a benign proliferation or a malignant cancer. Treatment and prognosis hinge upon this crucial distinction. Many breast lesions, particularly papillary lesions and in situ cancers, can be very complex, and therefore a second opinion is often advisable. Only a pathologist can make these diagnoses.
- Type of Cancer. Cancers that occur in the breast may be in situ (pre-invasive), micro-invasive, or invasive, and there are many different types of invasive cancers. The carcinomas arise from epithelial (ductal) cells, whereas the sarcomas arise from the stromal cells. Within the carcinoma group, most are ductal carcinoma; however, there are a variety of specific subtypes that have either better or worse prognoses. While the pathology can look similar between the different types of cancer, the treatment for these subtypes may be very different.
- Hormone Receptor Status and Her2/Neu Expression. Accurate assessment of ER, PR and Her2/Neu expression in a breast cancer is essential to determine whether the patient will benefit from hormonal therapy or anti-Her2 therapy, as well as predict overall patient outcome. Our full-service immunohistochemistry laboratory provides analysis of ER/PR expression, Her2/Neu overexpression, proliferation and other markers.
PATHOLOGY REPORT
SECOND OPINION OF PATHOLOGY REPORTS IN NODE-NEGATIVE BREAST CANCER PATIENTS - RATES OF CHANGE ARE "SIGNIFICANT"
In the Kennecke HF et al. 2012 study, 405 breast cancer estrogen-positive, node-negative breast cancer patients had a second opinion on their pathology report.
"A total of 102 pathology changes were documented among 81 patients (20%), The most frequently changed elements were grade (40%) and lymphovascular (26%), nodal (15%), and margin (12%) status. These changes results in 27 treamtne modification among 25 patients (6%). Treatment changes were primarily related to nodal and margin status, and only two of 27 were related to meansurement of tumor biology in women with estorgen and receptor-positve, node-nagative breast cancer."
Interestingly, the researchers commented, "In breast cancer, secondary pathology review may have the greatest chance of optimizing treatment regimens when applied to patients with ductal carcinoma in situ (DCIS) or node-negative breast cancer. Review of DCIS may identify invasive disease or suggest that the lesion is an atypia, falling short of a diagnosis of DCIS. Node-negative breast tumors are reviewed to verify pathologic nodal status; histologic characteristics such as grade, size, and presence of lymphatic or vascular invasion; and status of biomarkers. Because not all patients with node-negative disease are offered chemotherapy or postmastectomy radiation, a change in pathology may result in a significant change in therapy."
Conclusion: "Reported rates of change are significant and warrant routine secondary pathology review among patients with node-negative breast cancer or ductal carcinoma in situ before final treatment is recommended. Review remains relevant in the era of gene expression signatures to determine margin and nodal status."
(See Kennecke HF et al., Impact of Routine Pathology Review on Treatment for Node-Negative Breast Cancer, J Clin Oncol, 2012.)
PATHOLOGY REPORT
MORE ON "ERA OF GENE EXPRESSION" ALLUDED TO IN KENNECKE ET AL, STUDY ABOVE - 2016 ASCO GUIDELINES ON USING GENE EXPRESSION TO GUIDE TREATMENT
The objective of the Harris LN et al. 2016 was, "To provide recommendations on appropriate use of breast tumor biomarker assay results to guide decisions on adjuvant systemic therapy for women with early stage invasive breast cancer.
ASCO (American Society of Clinical Oncology Clinical Practice Recommendations:
"In addition to estrogen and progesterone receptors and human epidermal growth factor receptor 2, the panel found sufficient evidence of clinical utility for the biomarker assays Oncotype DX, EndoPredict, PAM50, Breast Cancer Index, and urokinase plasminogen activator and plasminogen activator inhibitor type 1 in specific subgroups of breast cancer. No biomarker except for estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 was found to guide choices of specific treatment regimens. Treatment decisions should also consider disease stage, comorbidities, and patient preferences."
( See Harris LN et al., Use of Biomarkers to Guide Decisions on Adjuvant Systemic Therapy for Women with Early-Stage Invasive Breast cancer: American Society of Clinical Oncology Clinical Practice Guideline, 2016)
EXAMPLE OF BIOMARKER ASSAY - ONCOTYPE DX
"SUFFICIENT UTILITY" - NOT TO GUIDE CHOICES OF "SPECIFIC TREATMENT REGIMENS" - ONCOTYPE DX.
"The Oncotype DX breast cancer test works by examining a sample of breast cancer. The test measures a group of breast cancer genes in this sample to see how active they are (also known as how they are expressed). The result of the test is reported as a number between 0 and 100, known as the Recurrence Score® result. A lower score means the cancer has a lower chance of returning, and a higher score means that there is a higher chance of the cancer returning. The score also provides patients and doctors with important information regarding the potential benefit of adding chemotherapy to hormonal therapy. A low score indicates that the patient will receive minimal benefit from chemotherapy, whereas a patient with a high score can have significant benefit from chemotherapy. Because everyone's body and tumor are unique, obtaining a Recurrence Score result helps make treatment decisions tailored to you.
The Oncotype DX breast cancer test provides information in addition to standard measurements (such as tumor size, tumor grade and lymph node status) that doctors have traditionally used to estimate how likely a patient's cancer is to return, and to help make treatment decisions."
)See http://breast-cancer.oncotypedx.com/en-US/Patient-Invasive/WhatIsTheOncotypeDXCancerTest.aspx.)
PATHOLOGY REPORT
SO, YOUVE HAD SURGERY - NOW YOU WANT INDIVIDUALIZED CANCER THERAPY. THERE MIGHT BE PROBLEMS! TESTING FOR MUTATIONS IN TUMORS MIGHT BE MISLEADING IN ALMOST HALF OF CANCER PATIENTS - SERIOUS IMPLICATIONS FOR
TARGETED THERAPY
Here is a wonderful summary of the Jones S et al. 2015 study on the analysis of tumors for mutations in Science Translational Medicine, which is humorously entitled, Will the Real Mutation Please Stand Up?
Will the Real Mutation Please Stand Up? (From Science Translational Medicine.)
"When a patient is diagnosed with cancer, a sample of the tumor is often analyzed to look for mutations that may guide the approach to targeted treatment of the disease. Jones et al. analyzed samples from more than 800 patients with 15 different cancer types and showed that this standard approach is not necessarily accurate without also analyzing a matched sample of normal DNA from the same patient. The authors found that, compared to analysis of paired samples, the standard tumor-only sequencing approach frequently identified mutations that were present in the patient's normal tissues and were therefore not suitable for targeted therapy or, conversely, missed useful mutations in the tumor."
Excerpts From Science Daily: In the Jones S et al. 2015 study, the researchers examined the germline (normal tissue) and tumors (from different cancers, including breast cancer) for mutations as a prelude to devising targeted therapy strategies. This process that led the researchers to discover that "sequencing tumor genomes for clues to genetic changes might misdirect treatment in nearly half of all patients unless it is compared first to a genetic readout of their noncancerous tissue."
The researchers examined normal and cancerous tissues for variations: "When the researchers only looked at the genetic changes found in a patient's tumor and filtered out the most well-known germline changes, they counted 382 possible tumor-related changes. But after comparing a patient's full germline genome to his or her tumor genomes, they determined that, on average, 249 of these changes were part of the patient's normal, inherited genetic variation and were not tumor-specific. In other words, researcher, Victor Velculescu, M.D., Ph.D., says, 65 percent of the genetic changes identified with tumor-only genetic sequencing were 'false positives' and not related to the patient's cancer."
How about actionable genes? "The researchers also looked at changes in 'actionable genes,' or genes for which some kind of drug or cancer therapy has already been identified. When they looked for these changes in the tumor alone, they identified on average 2.4 changes per patient. However, they found that 33 percent of those changes were also false positives when they compared the tumor genome to the patient's germline genome. These false positives affected 48 percent of the patients analyzed."
Thus, " 'In tumor-only analyses, we found that nearly half of patients had tumor mutations that were actually germline or false positives in actionable genes, and they could lead to inappropriate therapy,' Velculescu says."
From the study: The researchers' observations suggest that " a high fraction of human tumors have alterations that may be clinically actionable and that a small but notable fraction of apparently sporadic cancer patients have pathogenic germline changes in cancer-predisposing genes. Additionally, these data support the notion that accurate identification and clinical interpretation of alterations benefit from analysis of both tumor and normal DNA from cancer patients."
(For the study, see Jones S et al., Personalized Genomic Analyses for Cancer Mutation Discovery and Interpretation, Sci Trans Med, 2015. ... For the Science Daily Article, see http://www.sciencedaily.com/releases/2015/04/150415155108.htm.... For the summary, Will the Real Mutation Please Stand Up?, http://www.sciencemag.org/content/348/6232/298.8.full, 2015.)
PATHOLOGY
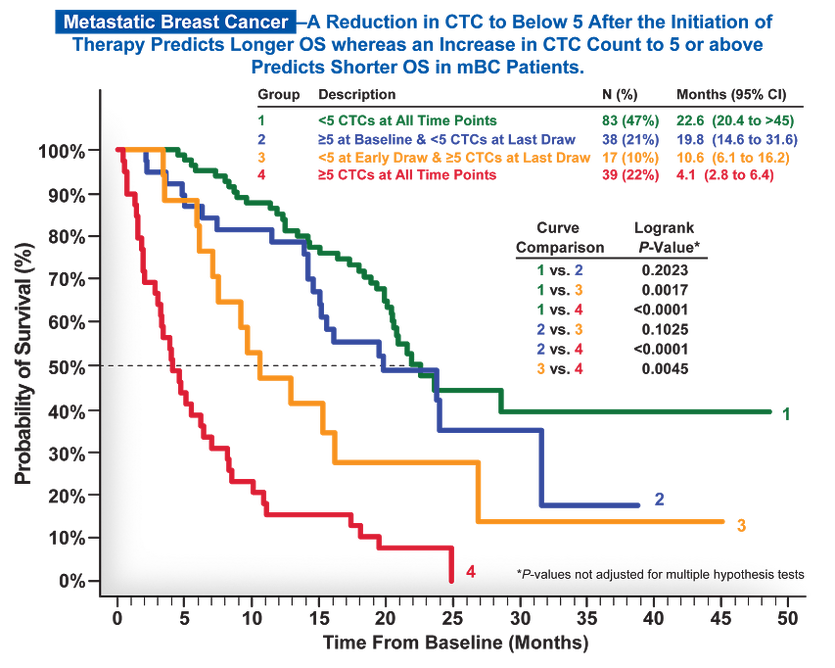
LOOKING NOT AT THE TUMOR, BUT THE BLOOD - CIRCULATING TUMOR CELLS IN EARLY BREAST CANCER - A "PROGNOSTIC BIOMARKER"
What are circulating tumor cells?
"Circulating tumor cells are cells that have shed into the vasculature from a primary tumor and circulate in the bloodstream, CTCs thus constitute seeds for subsequent growth of additional tumors (metastasis) in vital distant organs, triggering a mechanism that is responsible for the vast majority of cancer-related deaths."
wikipedia.org
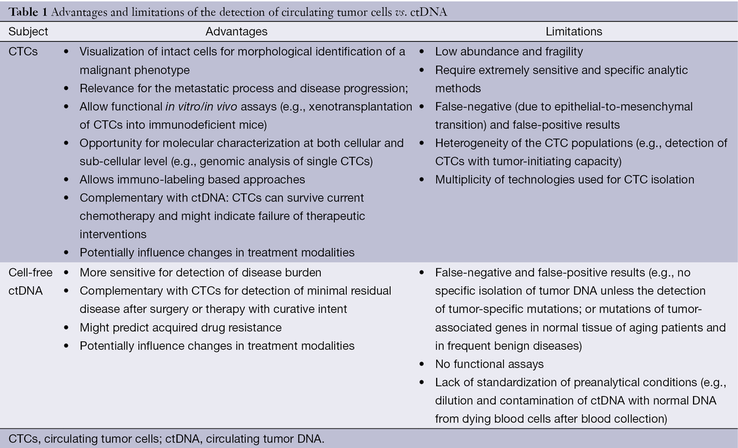
"CTC detection proved to be a significant prognostic factor in both early and metastatic BC, but evidence supporting its clinical utility are still expected through numerous ongoing trials. While ctDNA (Note: DNA fragments from dead or dying cancer cells) is apparently a better material for the characterization of the cancer mutational landscape (Alix-Panabieres and Pantel, 2013; Bidard et al., 2013a), the intrinsic biological role of CTC as metastatic 'seeds' and its corresponding clinical prognostic impact guarantee the use of CTC as a major biological and clinical tool in BC patients."
Bidard F-C et al., Circulating Tumor Cells in Breast Cancer, Science Direct, 2016.
Bidard F-C et al., Circulating Tumor Cells in Breast Cancer, Science Direct, 2016.